An impactful yet little understood opportunity for payers to improve member health outcomes crystallized on August 18, 2017, when President Trump signed into law the Over-the-Counter (OTC) Hearing Aid Act. For decades, hearing care has languished on the periphery of the U.S. healthcare system, with hearing aids covered neither by Medicare nor most private insurers and the devices priced out of reach for most Americans. The OTC Act, however, by bringing to market approved, reasonably priced hearing devices, will enable payers to create a new model of hearing care—crucial because hearing loss is often the missing link to members’ health.
By 2020, close to 45M people in the United States will suffer from hearing loss, with 40M of them over 50. Yet less than 20% of Americans who would benefit from hearing aids wear them. One cause: the $4,600 average price tag for a pair of hearing aids. Also driving the low adoption rate is lack of payer focus, translating into lackluster physician screening rates for hearing loss. Less than a quarter of adults aged 20 to 69 had a hearing examination in the last five years, compared with over half of patients 18 years plus who were screened for vision problems in the last two years.
“Payers ignore hearing loss at the peril of their members’ health.”
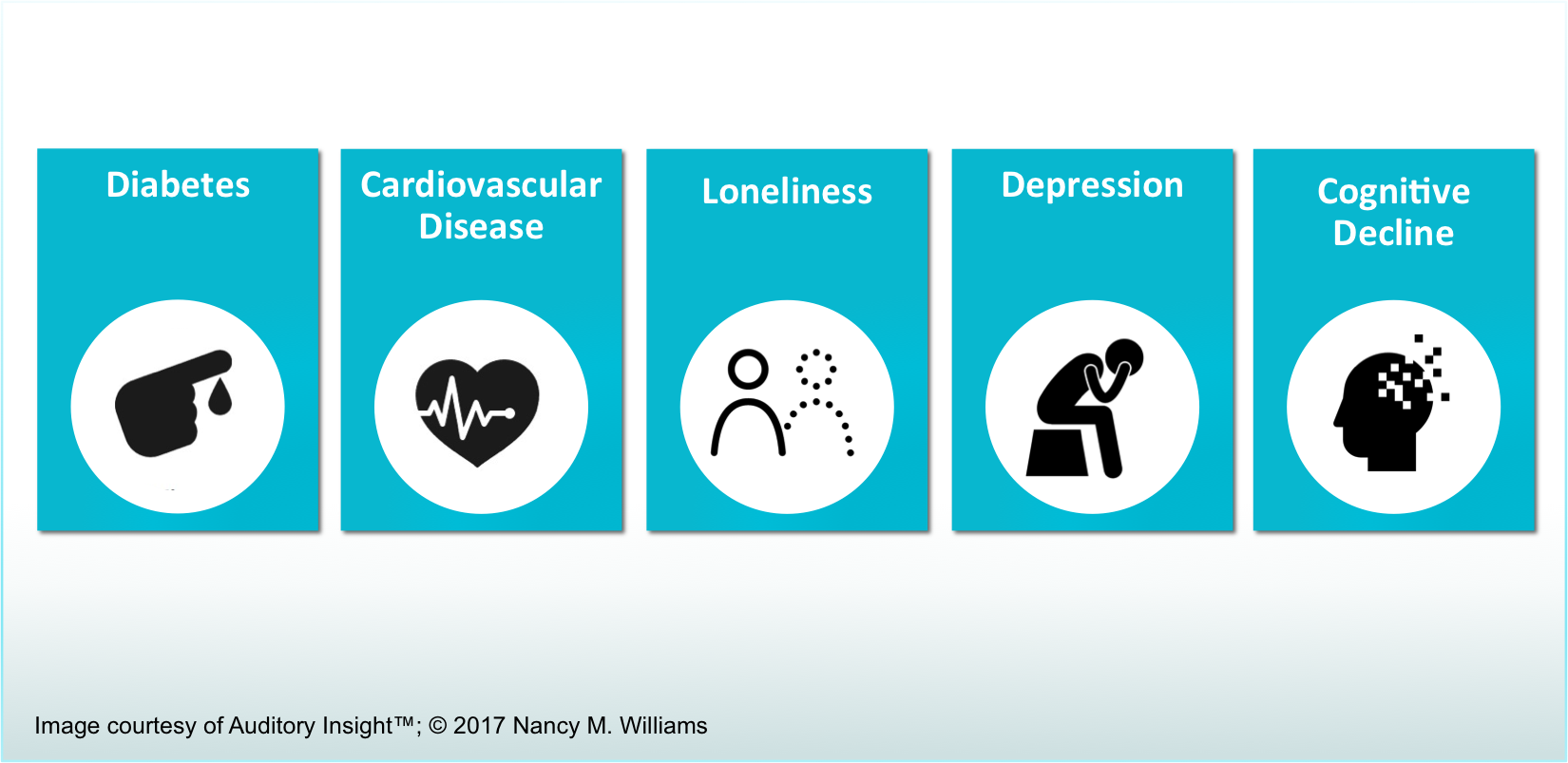
But payers ignore hearing loss at the peril of their members’ health. Hearing loss is correlated with psychosocial conditions of loneliness, depression, and cognitive decline. Research shows that wearing hearing aids reduces perceptions of loneliness and symptoms of depression. The Lancet reports that interventions for hearing loss and eight other key risk factors may delay or prevent a third of dementia cases.
Addressing hearing loss also has the potential to improve existing chronic care programs for diabetes and cardiovascular disease, both correlated with hearing loss. These chronic care programs emphasize improvements in diet and exercise. But members with untreated hearing loss, who struggle to hear instructors and friends in exercise programs ranging from aerobics classes to neighborhood walks, have less motivation to stick with their goals. Since patients usually deign to mention their hearing loss to medical practitioners—the stigma against hearing loss is overpowering for many—payers do not have a clear window into how to improve the health of patients with undiagnosed hearing loss.
The OTC Act, a provision of the Food and Drug Administration (FDA) Reauthorization Act, directs the FDA to create a new class of OTC hearing aids for adults with mild to moderate loss. Press coverage of the new law focuses on how reasonably priced hearing aids will become directly available to consumers online and in drugstores. Retail prices of no more than $500 a pair are reasonable to expect.
“The emergence of these devices offers an opportunity to create a new framework of hearing care.”
For payers, however, the emergence of these devices offers an opportunity to create a new framework of hearing care. The devices’ significantly lower prices, combined with their benefits to the patient’s entire health, tips the cost-benefit balance towards fully covering a pair of $500 hearing aids.
Payers should enlist primary care physicians as the first line of defense in diagnosing hearing loss. Physicians may use the NTID Speech Recognition Test, a statistically significant proxy for an audiogram administered in a soundproofed booth, to diagnose patients with a mild to moderate loss. Payers should include hearing testing as an explicit metric in their value-based contracts with physician networks. Routine hearing testing and coaching on wearing hearing aids should become a standard component of chronic care management programs for conditions like diabetes and cardiovascular disease that are correlated with hearing loss.
Covering hearing care is simply good medical policy. Now is the time for payers to monitor how the FDA will shape the OTC guidelines and to begin planning changes in their processes to bring hearing care from the periphery of the U.S. healthcare system into the mainstream.

Leave A Comment